Diabetes is an illness that is difficult to manage and complicated, and it affects millions of individuals all over the world. Beyond the immediate concerns related to blood sugar control, individuals with diabetes often face additional health issues. Additionally, Fill out this form to check if you or a friend qualify for CGMs.
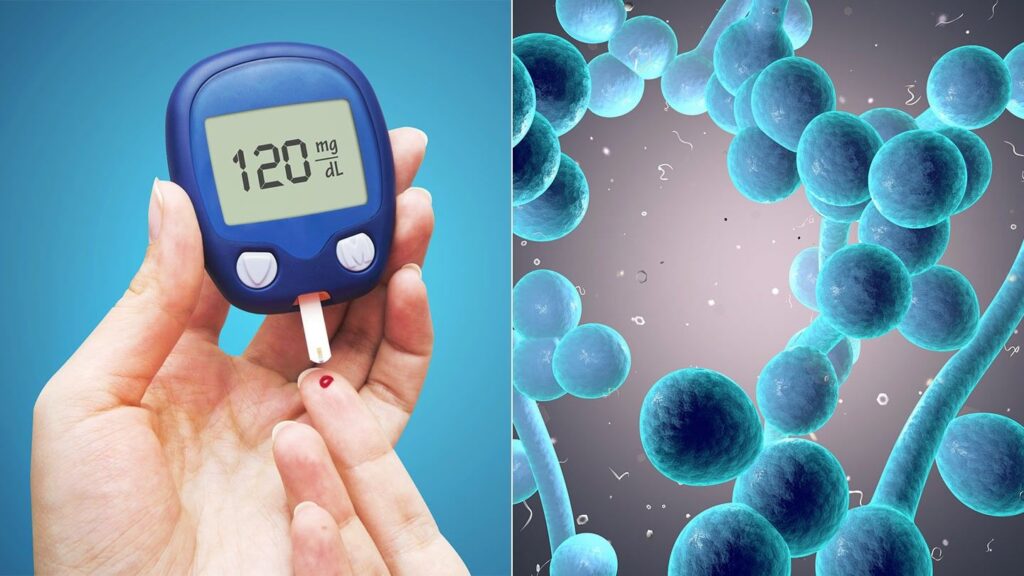
One such issue is the increased risk of yeast infections. Understanding the connection between yeast infections and diabetes, as well as effective management strategies, is crucial for maintaining good health.
The Link Between Diabetes and Yeast Infections
Yeast infections, particularly candidiasis, are more common in individuals with diabetes. This increased susceptibility is primarily attributed to the altered environment within the body due to diabetes. Let’s delve into the factors that connect these two conditions.
1. Elevated Blood Sugar Levels
High blood sugar levels, a hallmark of diabetes, provide an ideal environment for the overgrowth of yeast, particularly Candida species. Yeast thrives on sugar, and excess glucose in the bloodstream can lead to an imbalance that promotes yeast proliferation. This is why individuals with poorly controlled diabetes are at a higher risk of yeast infections.
Read Guide about Wegovy Dosage Guide: The Best Way For Weight Loss
2. Weakened Immune System
Diabetes can weaken the immune system’s ability to combat infections effectively. Chronic high blood sugar levels can impair the function of white blood cells, which play a crucial role in the body’s defense against pathogens. With a compromised immune system, the body may struggle to control the growth of yeast, allowing it to multiply and cause infections more easily.
3. Altered Microbiome
The human body hosts a diverse community of microorganisms, including bacteria and yeast, that make up the microbiome. Diabetes can disrupt this delicate balance. When the balance of beneficial bacteria is disturbed, it can pave the way for yeast to thrive. This imbalance in the microbiome is particularly common in individuals with poorly controlled diabetes.
Must Read CGMs in noncritical care hospitals optimizes glycemic control
Common Types of Yeast Infections in Diabetes
Yeast infections can manifest in various forms, affecting different parts of the body. Here are some of the most common types of yeast infections in individuals with diabetes:
1. Genital Yeast Infections:
Genital yeast infections, also known as vulvovaginal candidiasis, are more prevalent in women with diabetes. In addition to itching and burning, patients may also experience a thick, white discharge.
2. Oral Thrush:
The yeast infection known as oral thrush can affect both the mouth and the throat. It can cause white, creamy lesions on the tongue, inner cheeks, and the back of the throat. It is more common in individuals with uncontrolled diabetes and those who use inhaled corticosteroids.
3. Skin Infections:
Yeast can also cause skin infections, leading to red, itchy, and sometimes painful rashes in areas where skin meets skin, such as under the breasts, in the groin, or between the toes.
4. Nail Infections:
Yeast infections can affect the nails, leading to brittle and discolored nails. This condition is more common in individuals with poorly controlled diabetes.
Managing Yeast Infections in Diabetes
Effective management of yeast infections in diabetes involves a multifaceted approach, focusing on both blood sugar control and infection treatment. Here are some strategies to consider:
1. Blood Sugar Control:
Maintaining good blood sugar control is paramount in preventing yeast infections. Monitoring your blood glucose levels regularly, adhering to your diabetes management plan, and following a healthy diet can help prevent the conditions that foster yeast overgrowth.
2. Medications:
When a yeast infection occurs, antifungal medications prescribed by a healthcare professional are typically the primary treatment. These medications come in various forms, including creams, ointments, oral tablets, or suppositories, depending on the type and location of the infection.
3. Topical Remedies:
In addition to prescribed medications, natural remedies like yogurt, coconut oil, or tea tree oil may provide relief from itching and discomfort. However, consult your healthcare provider before using these remedies.
4. Hygiene and Lifestyle Adjustments:
Maintaining good personal hygiene is essential to prevent and manage yeast infections. Avoid using harsh soaps or douches that may disrupt the balance of the vaginal or genital microbiome. Wearing breathable, cotton underwear and practicing good hygiene in skinfold areas can reduce the risk of skin yeast infections.
5. Probiotics:
Probiotics, which contain beneficial bacteria, may help restore the balance of the microbiome. Consult your healthcare provider to determine if probiotics are suitable for you.
Also, read about: Nocturnal Itching in Diabetes
Prevention is Key
Preventing yeast infections is often more manageable than treating them. If you have diabetes, consider the following preventive measures:
1. Blood Sugar Control: Maintain healthy blood sugar levels through regular monitoring and adherence to your diabetes management plan.
2. Personal Hygiene: Practice good personal hygiene, especially in areas prone to yeast infections, like the genitals, skinfold regions, and the mouth.
3. Diet: Consume a balanced diet that limits excessive sugar and refined carbohydrates, which can fuel yeast growth.
4. Medication Adjustments: If you are taking medications that increase the risk of yeast infections (such as corticosteroids or antibiotics), discuss potential alternatives with your healthcare provider.
5. Regular Checkups: Regular healthcare checkups can help identify and address diabetes-related complications, including yeast infections, at an early stage.
Conclusion
The connection between yeast infections and diabetes is a complex one, but understanding the factors that contribute to this relationship is crucial for individuals living with diabetes.
By focusing on blood sugar control, maintaining good hygiene, and seeking prompt treatment when necessary, individuals can effectively manage and reduce the risk of yeast infections.
Prioritizing diabetes management and overall health can lead to a higher quality of life and a reduced risk of complications. Always consult with healthcare professionals for personalized guidance and treatment.