Pioneering Diabetes Reversal without Immunosuppression
A groundbreaking discovery emerges as researchers implant a thread-like device harboring insulin-secreting pancreatic cells under-skin Implant, successfully reversing type 1 diabetes in mice without the necessity of anti-rejection medications. This innovation presents a potential alternative to the lifelong regimen of insulin injections for managing this condition.
Understanding Type 1 Diabetes and Under-Skin Implant Offers Hope
Type 1 diabetes manifests when the body’s immune system targets and destroys the insulin-producing cells within the pancreas, impeding insulin secretion. This necessitates a lifelong reliance on insulin injections or the use of insulin pumps for maintaining blood sugar levels.
Tip: Please fill out the form if you or a friend would like more information on CGMs.
A Collaborative Breakthrough
Researchers from Cornell University and the University of Alberta joined forces to pioneer an implantable device that secretes insulin while evading immune reactions often associated with implanted devices.
Minglin Ma, one of the study’s corresponding authors, highlighted the urgency in translating this innovation into practical, impactful solutions for individuals affected by type 1 diabetes, particularly children.
Must Read CGMs in noncritical care hospitals optimizes glycemic control
The Evolution of Implantable Solutions
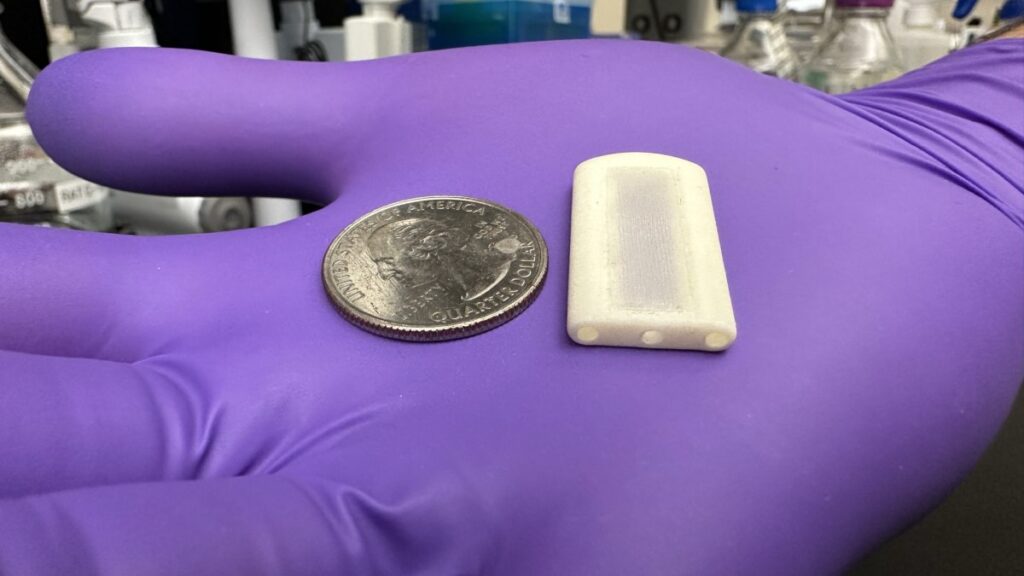
The initial development, Thread-Reinforced Alginate Fiber For Islets enCapsulation (TRAFFIC) in 2017, provided a foundation. Building on this, a more robust version emerged in 2021, demonstrating effective blood sugar control in mice for up to six months.
A Synergistic Approach for Enhanced Outcomes
The attention-grabbing success of Ma’s implant piqued the interest of diabetes researcher James Shapiro from the University of Alberta.
Shapiro’s method involved inserting islet cells under-skin implant channels and administering immunosuppression to safeguard them. The collaboration resulted in the creation of SHEATH, or Subcutaneous Host-Enabled Alginate THread.
Read Guide about Wegovy Dosage Guide: The Best Way For Weight Loss
Advancing the Implantation Technique
The SHEATH implantation involves a two-step process: inserting a nylon catheter under-skin to induce a controlled inflammatory response, forming a network of blood vessels.
Subsequently, the alginate-based islet cell-seeded device is placed within the created pocket, benefiting from the surrounding vessels’ oxygen and nutrient supply.
Promising Results and Future Challenges
Implanting the SHEATH system in diabetic mice showcased promising results, reversing the condition without immunosuppression. Demonstrating robust long-term potential, some mice maintained corrected blood glucose levels for over 190 days.
However, challenges remain, including sustaining long-term cell functionality and identifying suitable anatomical sites for placement.
Also, read about Semaglutide’s Impact on Non-Diabetic Obesity
Paving the Way for Future Solutions
Acknowledging these challenges, researchers are exploring solutions, including integrating continuous oxygen supply into the device.
Ma’s spin-off venture, Persista Bio, aims to develop a separate device to provide additional oxygen support to the cells, envisioning future versions of the implant lasting two to five years before replacement.
Despite hurdles, this pioneering research instills hope for a transformative solution, aiming to revolutionize diabetes management and offer sustained relief to individuals grappling with type 1 diabetes.