In the realm of diabetes management, the Glucose Management Indicator (GMI) has long served as a crucial metric for assessing blood sugar levels and guiding treatment strategies. However, with advancements in technology and a deeper understanding of diabetes, questions arise: Is it time to reconsider the relevance and efficacy of the Glucose Management Indicator? Let’s delve into this topic to understand the evolving landscape of diabetes care.
Understanding Glucose Management Indicator
The Glucose Management Indicator, commonly referred to as GMI, provides an estimation of average blood glucose levels over a certain period. It is calculated based on the measurement of glycated hemoglobin (HbA1c), a marker that reflects blood sugar levels over the preceding 2-3 months. Traditionally, healthcare providers have relied on GMI to assess long-term glycemic control in individuals with diabetes.
Challenges with Glucose Management Indicator
While GMI has been a valuable tool in diabetes management, it is not without limitations. One significant challenge is its inability to capture short-term fluctuations in blood sugar levels, which can be crucial for making immediate treatment adjustments. Additionally, factors such as variations in red blood cell lifespan and certain medical conditions can affect the accuracy of GMI readings, leading to potential misinterpretations of glycemic control.
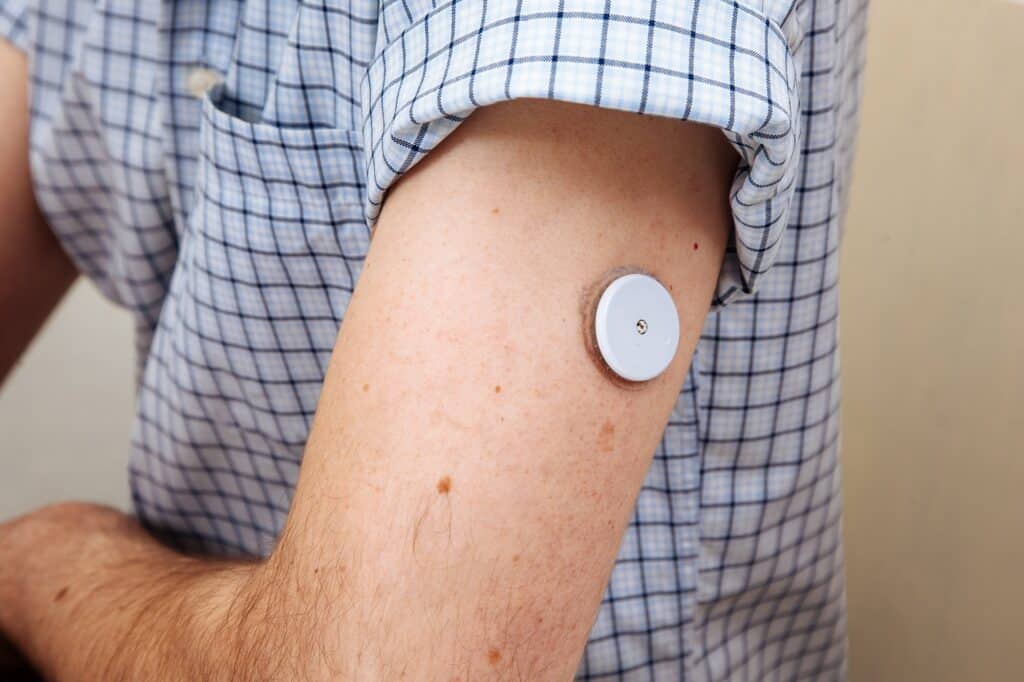
The Rise of Continuous Glucose Monitoring (CGM)
In recent years, the landscape of diabetes care has been revolutionized by Continuous Glucose Monitoring (CGM) technology. CGM devices provide real-time data on glucose levels, offering a comprehensive picture of glycemic patterns throughout the day and night. Unlike GMI, which offers a retrospective view, CGM enables proactive management by identifying trends, detecting hypoglycemic and hyperglycemic episodes, and guiding lifestyle modifications and medication adjustments in real time.
Must Read Is Dexcom Stelo Redefining Glucose Monitoring for Type 2 Diabetes?
The Role of Time in Range
As CGM technology becomes increasingly integrated into diabetes management, the concept of Time in Range (TIR) has gained prominence. TIR represents the percentage of time spent within a target range of blood glucose levels, typically defined as 70-180 mg/dL. Unlike GMI, which focuses solely on average glucose levels, TIR provides insights into the variability and stability of blood sugar control, offering a more nuanced assessment of glycemic management.
Rethinking Diabetes Care
Given the limitations of the Glucose Management Indicator and the advancements in continuous glucose monitoring technology, there is growing debate within the medical community about the need to rethink traditional approaches to diabetes care. While GMI remains a valuable tool for assessing long-term glycemic control, its role may need to be supplemented or even supplanted by metrics such as Time in Range to provide a more comprehensive and dynamic assessment of blood sugar management.
Also, read about Why are Continuous Glucose Monitors Essential for Diabetic Health?
Implications for Patient Care
The transition from GMI-centric to a more holistic approach incorporating CGM and Time in Range metrics carries significant implications for patient care. Healthcare providers must adapt their practices to leverage the insights offered by continuous glucose monitoring technology, empowering patients with real-time data and personalized treatment strategies. By embracing these advancements, we can enhance the precision and effectiveness of diabetes management, ultimately improving patient outcomes and quality of life.
Conclusion
As we navigate the evolving landscape of diabetes care, it is essential to critically evaluate the role of existing metrics such as the Glucose Management Indicator, and embrace innovations that offer a more comprehensive understanding of glycemic control. While GMI has been a cornerstone of diabetes management, the rise of continuous glucose monitoring technology and the emergence of Time in Range metrics signal a paradigm shift in how we assess and address blood sugar management. By rethinking our approaches and leveraging the latest advancements, we can usher in a new era of precision medicine in diabetes care.