Personalized Nutrition for Diabetes Remission
Transforming Diabetes Management: Insights from the German Diabetes Society Conference
In the pursuit of managing type 2 diabetes, an unconventional yet impactful ally emerges—nutrition therapy.
Dr. Diana Rubin, Chief Physician at Berlin’s Vivantes Humboldt Hospital, unveiled staggering revelations during the German Diabetes Society’s fall press conference. The spotlight? Personalized nutrition’s incredible potential to drive diabetes remission.
Tip: Please fill out the form if you or a friend would like more information on continuous glucose monitoring devices.
The Crucial Link: Nutrition & Diabetes Remission
Dr. Rubin’s insights defy the trend of sidelining nutrition therapy due to modern medicine’s ascendancy. While medications surged, nutrition therapy lingered in the background, despite its proven capability to significantly delay diabetes onset.
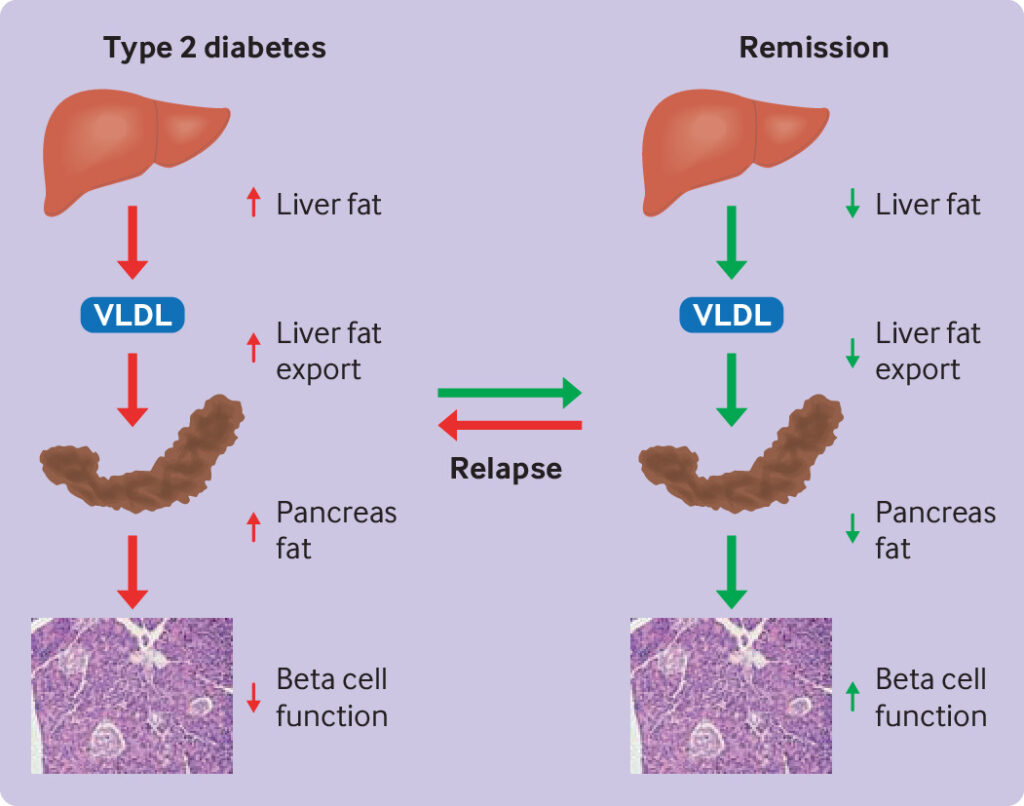
Despite these successes, sustained remission remains rare. Over five years, most patients relapse into type 2 diabetes, emphasizing the need for a personalized approach to nutrition therapy.
Redefining the Treatment Landscape
In the quest for effective diabetes management, the absence of coverage for personalized nutrition counseling by health insurance impedes progress. Current diabetes training, the only covered form of nutrition therapy, disregards the individualized needs crucial for diabetes care.
Contrary to this, studies like DiRECT showcase nutrition therapy’s prowess. Individualized approaches, coupled with constant therapist interaction, resulted in awe-inspiring remission rates exceeding 90%.
Must Read CGMs in noncritical care hospitals optimizes glycemic control
Telemedicine and Digital Support: A Paradigm Shift
Dr. Rubin emphasizes tailoring treatment to an individual’s lifestyle—a task accomplished best through personalized consultations. The key? Setting achievable goals, typically a 10% to 15% body weight reduction, and consistently monitoring progress for lasting results.
Adherence proves pivotal, and digital apps, particularly DiGAs, show promise in supporting patients’ objectives. The integration of telemedicine complements these efforts, ensuring continuous engagement and aiding short-term interactions.
Read Guide about Wegovy Dosage Guide: The Best Way For Weight Loss
The Visceral Fat Conundrum: Unraveling Prediabetes Remission
Prediabetes serves as a precursor to type 2 diabetes, signaling imminent health risks. However, the Prediabetes Lifestyle Intervention Study exposes a key player—abdominal fat. Reductions in visceral abdominal fat significantly impact remission rates, enhancing insulin sensitivity and reducing diabetes risk.
A New Therapeutic Paradigm: Focus on Diabetes Remission
Redefining therapeutic objectives, Dr. Reiner Jumpertz-von Schwartzenberg’s team emphasizes remission in prediabetes management. Aiming for specific markers—lower fasting blood glucose, 2-hour glucose, and A1c values—linked to weight loss and waist circumference reduction, amplifies remission chances.
Also, read about Clinical Trial of Baricitinib in Type 1 Diabetes Treatment
Forging a New Path: Cost-Effective Strategies
Dr. Jumpertz-von Schwartzenberg’s research delves into the cost-effectiveness of this strategy, aiming to sway payer support and revolutionize clinical practice.
In the pursuit of diabetes remission, personalized nutrition emerges as a transformative force. Its potential to reshape diabetes care demands attention, underscoring the need for individualized, holistic approaches in our fight against diabetes.