Lung Dendritic-Cell Metabolism
Abstract
People with diabetes suffer from a heightened vulnerability to respiratory viral infections, including influenza and SARS-CoV-2. However, the underlying mechanism behind this susceptibility remains unknown.
In this study, we utilized mouse models of diabetes, both acquired and genetic, to investigate the effects of hyperglycemia on lung dendritic cells (DCs).
We found that hyperglycemia impairs the expression of costimulatory molecules, antigen transport, and T cell priming in distinct subsets of lung Lung Dendritic-Cell Metabolism.
Tip: Please fill out the form if you or a friend would like more information on glucose monitors.
This leads to a defective antiviral immune response, delayed viral clearance, and increased mortality. Further analysis revealed that hyperglycemia induces alterations in Lung Dendritic-Cell Metabolism, including increased glucose-to-acetyl-CoA conversion and subsequent histone acetylation.
These metabolic changes cause global chromatin alterations and impaired expression of key Lung Dendritic-Cell Metabolism effectors involved in antigen presentation.
However, we discovered that glucose-lowering treatment and pharmacological modulation of histone acetylation can rescue Lung Dendritic-Cell Metabolism function and restore antiviral immunity.
In summary, our findings suggest that a hyperglycemia-driven metabolic-immune axis plays a pivotal role in Lung Dendritic-Cell Metabolism dysfunction during pulmonary viral infection. Targeting these metabolic checkpoints may hold therapeutic potential for mitigating severe viral disease in individuals with diabetes.
Don’t miss the Guide about Wegovy Dosage Guide: The Best Way For Weight Loss
Introduction
Diabetes mellitus is a major public health concern that is associated with various complications arising from the inability to maintain proper glucose control. One intriguing phenomenon observed in both type 1 and type 2 diabetes is the increased susceptibility to respiratory infections. This susceptibility leads to heightened morbidity and mortality when infected with viruses such as influenza.
Recently, the impact of diabetes on respiratory viral infections has become even more significant due to the COVID-19 pandemic. It has been observed that individuals with diabetes are more likely to experience severe outcomes, higher mortality rates, and are at increased risk of breakthrough infections even after vaccination.
Nevertheless, our understanding of the underlying mechanisms behind this susceptibility to respiratory infections in individuals with diabetes is limited.
Previous studies using animal models have explored this link, but a clear explanation for the increased risk has yet to be elucidated.
Therefore, we aimed to investigate the factors that contribute to the susceptibility of individuals with diabetes to pulmonary viral infections.
Must Read CGMs in noncritical care hospitals optimizes glycemic control
Impact of Diabetes on Viral Lung Disease
To assess the severity of the disease and immune responses, we examined hyperglycemic mice infected with the H1N1 influenza A virus. These mice exhibited progressively increasing levels of hyperglycemia and, similar to diabetic humans, showed significantly higher mortality rates compared to non-diabetic controls.
Furthermore, the hyperglycemic mice displayed elevated viral titers and reduced lymphocyte infiltration in the lungs, indicative of impaired viral clearance.
Interestingly, although the expression of interferon-beta (Ifnb1) and other antiviral proteins was augmented in hyperglycemic mice, suggesting an intact innate immune response, there was a significant reduction in the number of T cells and B cells involved in adaptive immunity.
This alteration in the adaptive immune response was accompanied by decreased production of antiviral antibodies. Notably, when blood glucose levels were normalized through insulin treatment, viral titers decreased, and the antiviral T cell and antibody responses were restored.
These observations indicate that hyperglycemia exacerbates viral lung disease and impairs lung’s ability to mount an effective adaptive immune response.
Also, read about Stem Cell Implants for Type 1 Diabetes
To confirm these findings, we employed a different model of hyperglycemia induced by the administration of streptozotocin (STZ), which causes acute hyperglycemia by destroying insulin-producing beta cells in the pancreas. Similar to the previous model, STZ-treated mice infected with the influenza virus exhibited enhanced mortality and increased viral titers compared to non-diabetic mice.
Notably, insulin supplementation in the diabetic STZ-treated mice restored viral clearance and improved adaptive immunity. Additionally, we investigated a type 2 diabetes model using leptin receptor-deficient (Db/Db) mice.
These mice spontaneously develop hyperglycemia, and upon infection with the influenza virus, they displayed higher mortality, elevated viral titers, and impaired adaptive immune responses.
Interestingly, unlike the type 1 diabetes models, the Db/Db mice exhibited hyperinsulinemia alongside hyperglycemia.
This suggests that the detrimental effects observed in this model are not directly related to insulin levels. Furthermore, we extended our investigation by infecting hyperglycemic Akita mice with the mouse pneumonia virus (PVM) and found similar results. These findings indicate that hyperglycemia in both type 1 and type 2 diabetes leads to impaired lung antiviral adaptive immunity, delayed viral clearance, and increased susceptibility to respiratory infections.
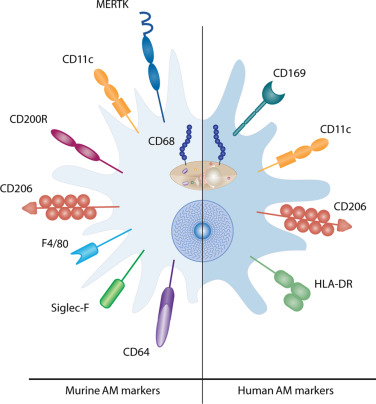
Altered Lung Dendritic Cell Composition in Hyperglycemia
To gain insights into the mechanisms underlying immune dysfunction and susceptibility to infection in hyperglycemia, we conducted single-cell RNA sequencing (scRNA-seq) of lung cells from hyperglycemic Akita mice and non-diabetic controls during both steady-state and acute influenza virus infection.
Through scRNA-seq analysis, we identified various cell types and states in the lungs. Interestingly, while influenza transcripts were detected in specific cell types such as alveolar and ciliated epithelial cells, macrophages, and others, Lung Dendritic-Cell Metabolism and lymphocytes did not show influenza gene expression.
We observed significant changes in the abundance and transcriptomic profiles of multiple pulmonary cell subsets during lung infection.
Specifically, new subsets of macrophages, Lung Dendritic-Cell Metabolism, natural killer (NK) cells, T cells, B cells, neutrophils, and fibroblasts emerged during infection.
Moreover, acute influenza infection induced substantial transcriptional responses in various immune cell subsets, including monocytes, macrophages, Lung Dendritic-Cell Metabolism, T cells, NK cells, and others. These findings indicate dynamic changes in lung cell subsets and transcriptional profiles during pulmonary viral infection.
Conclusion
In conclusion, our study provides insights into the mechanisms underlying the increased susceptibility to respiratory viral infections in individuals with diabetes.
We demonstrate that hyperglycemia impairs lung dendritic cell function, leading to defective antiviral adaptive immune responses, delayed viral clearance, and increased mortality.
Moreover, we uncover alterations in Lung Dendritic-Cell Metabolism driven by hyperglycemia, resulting in global chromatin modifications and impaired expression of key genes involved in antigen presentation.
Importantly, our findings offer hope for potential therapeutic interventions by showing that glucose-lowering treatment and pharmacological modulation of histone acetylation can rescue dendritic cell function and restore antiviral immunity.
By targeting the metabolic-immune axis, we may be able to mitigate the severe outcomes of viral infections in individuals with diabetes.