Investigating Hypoglycemia After Meals After Oesophagogastric Cancer Surgery
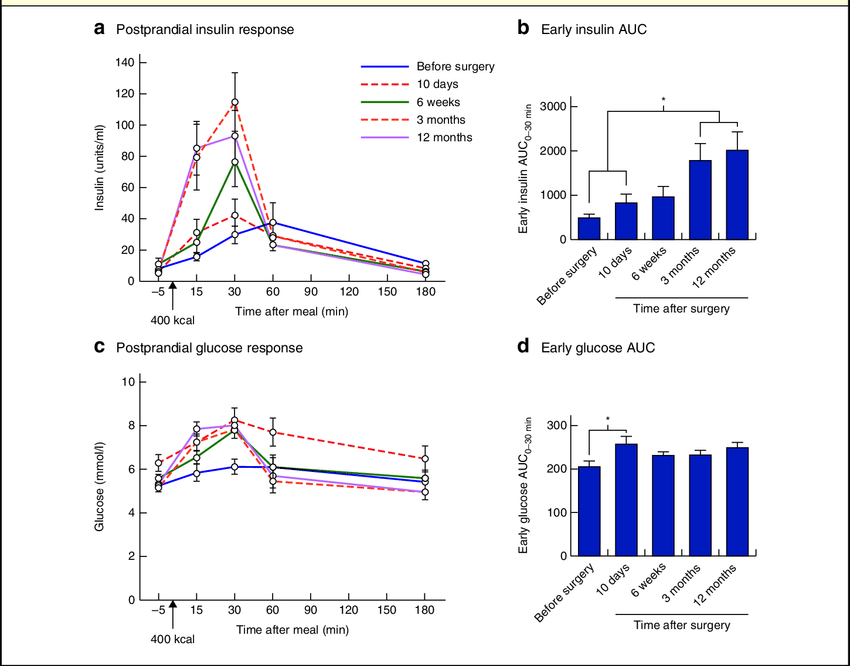
Postprandial hypoglycemia, occurring in a substantial percentage of patients following oesophagogastric cancer surgery, presents a significant challenge in managing glucose levels. The dysregulation is often attributed to an exaggerated incretin response post-meals, triggering an excessive insulin release that leads to low blood glucose levels.
The Role of Continuous Glucose Monitoring
Continuous glucose monitoring (CGM) systems have emerged as valuable tools in understanding and managing postprandial hypoglycemia. By providing real-time interstitial fluid glucose readings at regular intervals, CGMs offer insights into glycemic fluctuations, enabling patients and healthcare providers to identify patterns and triggers associated with hypoglycemic episodes. Please fill out the form if you or a friend would like more information on Continuous Glucose Monitors.
The utilization of a CGM system, such as the FreeStyle® Libre™ continuous glucose monitor, was pivotal in a pilot study involving patients post-oesophagogastric cancer surgery. This study aimed to monitor glycaemic profiles, detect hypoglycemic episodes, and evaluate the effectiveness of interventions in managing these episodes.
The Impact of Low-Glycemic Index Diet
In tandem with CGM utilization, the study implemented a tailored low-glycemic index (GI) diet as an intervention strategy. A low-GI diet involves consuming foods that induce slower glucose release, thus preventing rapid spikes in blood sugar levels. By prioritizing low-GI food options and moderating high-GI carbohydrates during meals, this dietary approach aims to mitigate insulin peaks and reduce the risk of postprandial hypoglycemia.
The study outcomes, albeit within a limited participant pool, showcased promising trends. Patients who followed the low-GI diet alongside CGM monitoring observed improvements in their glycemic profiles.
Despite no statistically significant differences in the pilot study, there was a notable reduction in the frequency of hypoglycemic episodes post-intervention.
Must Read CGMs in noncritical care hospitals optimizes glycemic control
Implications for Clinical Management
The study findings underscore the significance of continuous glucose monitoring in highlighting an often under-recognized aspect of post-oesophagogastric cancer surgery management.
Moreover, it sheds light on the challenges associated with hypoglycemia unawareness in these patients, emphasizing the critical need for education and resources focused on recognizing and managing postprandial hypoglycemic episodes.
Read Guide about Wegovy Dosage Guide: The Best Way For Weight Loss
Extending Intervention Strategies and Future Directions
While the low-GI diet demonstrates potential as an initial intervention, the study also acknowledges the need for alternative treatments in cases where hypoglycemia remains unresponsive.
Strategies involving α-glucosidase inhibitors, somatostatin analogues, or diazoxide might be considered in refractory cases. Additionally, the potential role of novel GLP-1 receptor antagonists holds promise for future research and intervention.
The study’s scope, although a crucial initial step, prompts further exploration and validation across larger participant groups. A broader study could provide more robust evidence on the effectiveness of the low-GI diet in managing postprandial hypoglycemia after oesophagogastric cancer surgery.
Also, read about Discovering Continuous Glucose Monitoring’s Diabetes Care Potentially
Concluding Thoughts
In conclusion, the intersection of continuous glucose monitoring and a low-glycemic index diet offers a promising avenue in understanding and managing postprandial hypoglycemia after oesophagogastric cancer surgery.
While preliminary, these findings pave the way for further research and underscore the significance of tailored interventions and education in improving the quality of life for individuals navigating this complex condition.